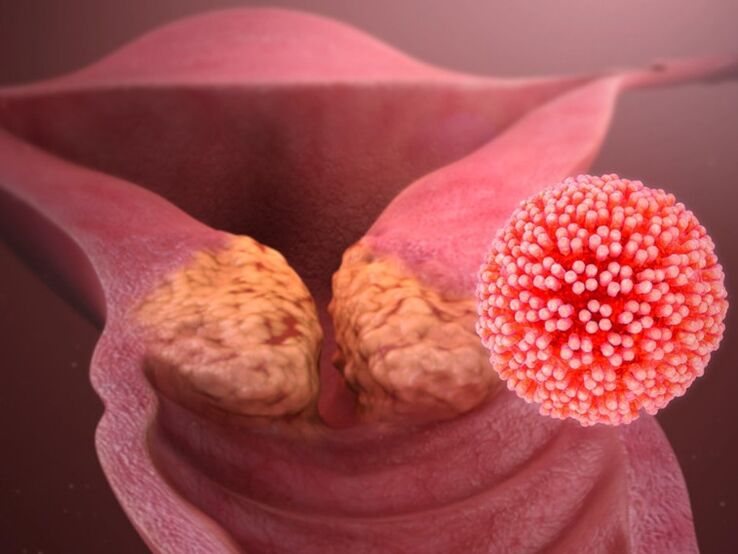
Human papillomavirus (HPV) provokes the development of papillomas, warts, warts and is a causative agent in the development of cervical and laryngopharyngeal cancers. Uncommonly, it may affect the oral mucosa, esophagus, eye conjunctiva. According to the World Health Organization, the incidence of this infection has increased 10-fold in the last 10 years. In our country, the prevalence of HPV infection in the region varies from 29% to 45%. The medical community is particularly cautious, as about a third of all isolated viral genotypes provoke the development of oncological pathology.
Classification of the course of papillomavirus infection
Once in a woman's body, HPV can show a variety of activities that depend on the state of immunity. Depending on the behavior of the pathogen, there are several variants of human papillomavirus infection:
- latent flow. The virus remains in the body but does not cause abnormal changes in the cells. No symptoms - the presence of the micro-organism can only be determined by molecular biological methods.
- HPV-Related Inflammation Usually we talk about cervicitis or vulvovaginitis on the background of HPV, which leads to a gynecologist. By consulting, she can learn: how to treat HPV in women. It should be understood that the virus does not cause inflammation per se, but creates the conditions for activating the inflammatory process.
- Condyloma, located in the anogenital region and on the mucous membranes of the genital tract, is a form of PVI (papillomavirus infection) that requires the use of modern surgical techniques to remove formations. After surgical removal, laser destruction, cryodestruction, or radioactive coagulation, complex treatment is required to prevent complications and relapses.
- Cervical dysplasia. May be asymptomatic or cause excretion. Severe forms of the disease are precancerous - to avoid this situation, a proper understanding of how HPV is treated in women is more important than ever.
Classification helps the doctor to choose the most effective treatment tactics. Pathogen strains are also divided into groups according to their ability to cause oncological diseases: HPV with high, medium and low oncogenic risk. Of the 40 sexually transmitted variants of the virus, 14 are classified as high and moderate oncogenic risk: -16, -18, -31, -33, -35, -39, -45, -51, -52, - 56, - 58, -59, -66 and -68 types.
How is the human papillomavirus transmitted?
In the female population, HPV infection reaches 70%. However, the presence of a pathogen in the body does not mean a disease. If a person has a healthy immune system, then HPV infection is in most cases transient - it goes away on its own within 2 years. If this does not happen, the question of how to treat the human papilloma virus in women becomes relevant.
The main route of virus transmission is contact:
- sexual;
- vertical (from mother to fetus during childbirth);
- household (using one towel, razor, underwear).
Young people between the ages of 13 and 30 are most susceptible to the virus infection. The risk of infection at the first sexual contact is about 60%. The virus can enter the body even in the absence of direct sexual intercourse. It is girls who are most at risk for HPV and then its consequences. This is due to the peculiarities of their genital structure.
Human papillomavirus in women: causes
In the female population, HPV infection reaches 70%. However, the presence of a pathogen in the body does not mean a disease. If a person has a healthy immune system, then HPV infection is in most cases transient - it goes away on its own within 2 years. If this does not happen, the question of how to treat the human papilloma virus in women becomes relevant.
- concomitant pathology of the reproductive system;
- endocrine disorders;
- immunodeficiency and beriberi;
- common acute infectious diseases - SARS, other viral and bacterial infections;
- early intercourse;
- abortion;
- smoking and alcohol consumption;
- chronic psycho-emotional stress that weakens the immune system;
- excessive physical and emotional stress, irregular daily routine;
- postpartum period - due to stress and hormonal changes;
- long-term use of immunosuppressive drugs and oral contraceptives.
Frequent changes in sexual partners also increase the risk of both becoming infected with new strains of the virus and activating an existing infection. When immunity is reduced, the virus is integrated into the genome of cells, which poses a high chance of cancer - how to cure HPV in women at this stage of medical science has not yet been discovered. That is why it is so important to control the activity of the virus and to stimulate the immune system properly.
The first signs of HPV in women and additional symptoms
The most obvious sign of the presence of HPV in a woman's body is the appearance of papillomas on the genital mucosa and skin of the anogenital region. They do not cause pain and, as a rule, go unnoticed for a long time. However, the virus can cause other unpleasant symptoms, which will prompt the woman to see a gynecologist immediately:
- abnormal vaginal discharge accompanied by itching and burning;
- frequent recurrence of vaginitis, bacterial vaginosis;
- vaginal discharge.
During the examination, the doctor sees benign formations on the skin, changes in the cervical epithelium, and signs of inflammation. Cancer can only appear in the later stages of a chronic papillomavirus infection.
Is it possible to cure the human papilloma virus?
To understand how HPV is currently treated in women, it is important to understand the approaches available to treat human papillomavirus infection. At present, treatment for HPV infection is reduced to the following:
- Preventing the progression of HPV infection;
- elimination of clinical manifestations;
- stimulation of systemic and local antiviral immunity.
There is no medicine that leads to the complete disappearance of the virus from the body. However, research in this area is ongoing, with doctors focusing on the need for combination treatment for different types of HPV. Genetic engineering research is promising. Scientists are considering "rewriting" the virus's code to destroy it rather than spread it. Reducing virus copies restores local immunity and prevents chronic inflammation.
Information for physicians on "How to treat HPV in women" is currently detailed in current clinical guidelines.
When is it necessary to visit a doctor?
Women should have a preventive examination by a gynecologist at least once a year. The need to see a doctor also arises if you experience any disturbing symptoms:
- neoplasms in the genital area;
- warts on other areas of the skin and mucous membranes;
- lower abdominal pain;
- unusual discharge or bad smell from the vagina;
- itching, swelling, redness of the genitals.
In case of accidental sexual intercourse, it is recommended to visit a gynecologist. He will have a test, take a gynecological smear and scrape to detect HPV.
If papillomas appear in other parts of the body, a dermatovenerologist should be consulted. When a papilloma or warts grow in the anus, intervention by a proctologist may be needed. This will help to determine treatment tactics and what remedies for the treatment of papilloma the patient should prescribe in a particular case for purchase at a pharmacy.
General treatment regimen
The primary weapon in the fight against HPV is man's own stable immunity. The American Center for Disease Control and Prevention draws attention to the fact that 90% of cases do not develop clinical contact with the virus because the virus is suppressed by innate immunity.
Treatment for HPV infection should be comprehensive and focus on:
- treatment of concomitant diseases;
- elimination of external manifestations of diseases - medically and, if necessary, surgically;
- reduction of viral load;
- stimulation of the body's own defenses.
Chronic psycho-emotional stress, poor environment and comorbidities reduce a woman's immune system's ability to cope with the virus on its own. There are medicines that have direct antiviral and immunomodulatory effects that help the body to strengthen and reduce the load on the virus. This modern medicine contains a spray of activated glycyrrhizic acid obtained from licorice root. This helps to stop the virus from multiplying early and reduces the number of copies of the HPV genetic material in the body. The device has a special intravaginal nozzle for inserting the drug into the cervix and distributing it evenly along the vaginal walls. Antiviral and immunomodulatory therapy during the latent course of papillomavirus infection may prevent the onset of unpleasant symptoms and the transmission of the infection to more aggressive forms. If the virus has caused changes in the genital area and cervical epithelium, the spray helps to:
- relieve inflammation;
- prevent itching;
- restore mucosal integrity;
- increase local immunity.
The product is also indicated during the preparation period for the removal of HPV-induced benign lesions to reduce viral activity and prevent relapse. The medicine helps to regenerate the skin and prevent secondary infections from attaching.
Removal of papillomas and warts
Benign formations caused by HPV are removed by the following methods:
- cryodestruction - exposure of the neoplasm to cold;
- electrocoagulation - high frequency current treatment;
- laser removal - laser irradiation in a layer until a scab appears;
- chemical destruction - treatment with special chemical solutions that are applied to the wart and destroy them;
- surgical removal - given the high risk of recurrence after this type of destruction, this is determined selectively - if no other method is possible.
One of the innovations in the treatment of HPV is the CRISPR / Cas9 system, which almost completely cuts the DNA and incorporates its sections, thus inactivating the spread of the virus.
Prevention
Barrier contraception (condoms) is recommended for primary prevention, which, although not an absolute protection against HPV, will reduce the level of exposure to the virus. You must be selective in choosing sexual partners. In case of accidental exposure, a special spray may be used to protect against HPV, herpes simplex virus and cytomegalovirus infection.
To date, HPV vaccination is the most effective. It protects against the most common and malignant types of human papillomavirus. In many countries, HPV vaccination is included in the mandatory immunization schedule. The best time to get vaccinated is in childhood and adolescence. It was previously thought that it would not make sense after 20 years of vaccination. However, recent studies show that HPV vaccination is appropriate and effective until the age of 45-47 years.
However, if a viral infection occurs, the task of secondary prevention is to maintain the patient's good health, especially the good state of his immune system. Women should see their gynecologist regularly for early detection of viral illness.














































































